What Is a Vaginal Yeast Infection?
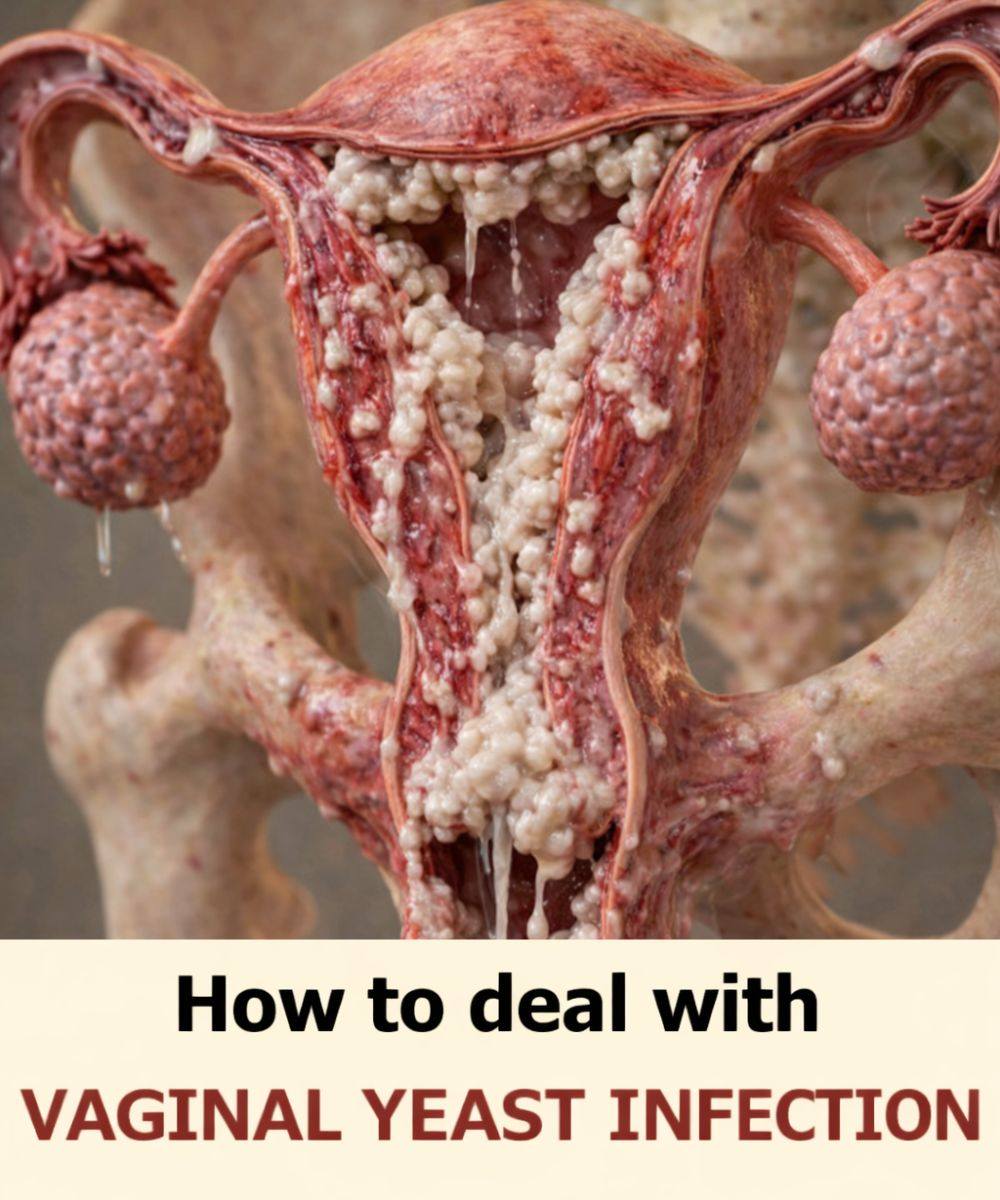
A vaginal yeast infection is caused by an overgrowth of a fungus called Candida, which normally lives in small amounts in the body. The vagina has a natural balance of yeast and bacteria. When that balance is disrupted, yeast can grow too quickly and cause symptoms.
Common symptoms may include:
Itching or irritation
Redness or swelling
Thick, white discharge
Burning or discomfort
These symptoms can vary in intensity and may come and go.
Why Yeast Infections Keep Coming Back
1. The Root Cause Was Never Fixed
Treatments often focus on stopping symptoms, not addressing why the imbalance happened in the first place. If the underlying trigger remains, yeast can return.
Common triggers include:
Changes in hormones
Certain medications
Lifestyle habits
Health conditions that affect the immune system
Without identifying the trigger, treatment may only offer temporary relief.
2. Antibiotic Use
Antibiotics kill harmful bacteria—but they can also kill beneficial bacteria that help keep yeast under control.
When good bacteria decrease:
Yeast has more room to grow
The vaginal environment becomes unbalanced
Some people notice yeast infections after even a short course of antibiotics.
What helps:
If antibiotics are necessary, supporting your body’s natural balance afterward can reduce the risk of recurrence.
3. Hormonal Changes
Hormones play a big role in vaginal health. Changes related to:
Puberty
Menstrual cycles
Hormonal birth control
Stress
can all affect the vaginal environment.
Higher estrogen levels can encourage yeast growth, which is why some people notice infections occurring at the same time each month.
4. Incomplete or Incorrect Treatment
Stopping treatment too early—even if symptoms improve—can allow yeast to survive and grow again.
Other issues include:
Using treatments that aren’t appropriate for your specific infection
Treating a condition that isn’t actually a yeast infection (some symptoms overlap with other conditions)
If symptoms return quickly, it may be a sign that treatment wasn’t fully effective.
5. Re-infection From the Environment
Yeast thrives in warm, moist environments. Certain habits can unintentionally support yeast growth, such as:
Wearing tight or non-breathable clothing
Staying in damp clothing for long periods
Using heavily scented soaps or hygiene products
These factors don’t cause yeast infections on their own, but they can make recurrence more likely.
6. Blood Sugar and Diet Factors
Yeast feeds on sugar. People with:
Frequent high blood sugar levels
Diets very high in added sugars
may be more prone to recurring infections.
This doesn’t mean sugar alone causes yeast infections, but it can contribute to an environment where yeast grows more easily.
7. A Weakened Immune System
Your immune system helps keep yeast under control. If it’s under stress—due to illness, lack of sleep, or ongoing stress—your body may have a harder time maintaining balance.
Even temporary immune changes can increase vulnerability.
What You Can Do to Help Prevent Recurrence
1. Get the Right Diagnosis
If infections keep returning, it’s important to confirm that symptoms are truly caused by yeast. Some other conditions can feel similar but require different care.
A healthcare professional can:
Identify the exact cause
Recommend appropriate treatment
Rule out other concerns
This step is especially important for repeated infections.
2. Complete All Treatments as Directed
Even if symptoms disappear early, finishing treatment helps ensure yeast is fully controlled. Stopping too soon increases the chance of recurrence.
3. Support Vaginal Balance Gently
Simple habits can make a big difference:
Choose breathable underwear
Avoid harsh or scented products
Keep the area clean with mild, unscented soap and water only on the outside
The vagina is self-cleaning; less intervention is often better.
4. Pay Attention to Patterns
Noticing when infections happen can be helpful. Ask yourself:
Do they occur after antibiotics?
Around the same time each month?
During periods of high stress?
Patterns can offer clues about triggers and help guide prevention.
5. Focus on Overall Health
ADVERTISEMENT